Lifespan and Clinical Biomechanics
We do
- Investigating aging, mild cognitive impairment, and neurodegenerative diseases, and uncovering how cognitive decline alters balance and motor-control strategies.
- Advancing pediatric biomechanics through studies on cerebral palsy (CP), developmental dysplasia of the hip (DDH), and Duchenne muscular dystrophy (DMD), yielding quantitative indicators for early diagnosis and intervention.
Journal Publication
[1] Wang, J.-Y., Lu, S.-H., Hu, C.-H., Wu, K.-W., Wang, T.-M., and Lu, T.-W.*(2025). Uphill walking unveils hidden instability and biomechanical adaptations in anterior cruciate ligament-deficient copers. Gait & Posture, 120: 110008. (SCI)
[2] Chang, C.-F., Lu, T.-W., Hu, C.-H., Wu, K.-W., Kuo, C.-C., and Wang, T.-M.* (2025). Lower limb inter-joint coordination and end-point control during gait in adolescents with early treated unilateral developmental dysplasia of the hip. Bioengineering, 12(8): 836. (SCI)
[3] Lu, S.-H., Kuan, Y.-C., Wu, K.-W., Wang, T.-M., and Lu, T.-W.* (2025). Cognitive-motor dual task induces strategic kinematic adjustments with increased toe-obstacle clearance for older adults during obstacle crossing. PLOS ONE. (SCI)
[4] Lu, Y.-L., Yu, C.-H., Wang, T.-M., & Lu, T.-W.* (2025). Immediate effects of monocular viewing on lower-limb joint and endpoint kinematics during obstructed gait in young and older adults. Gait & Posture. (SCI)
Projects
Development of a Tablet-Based System for Testing and Measuring Whole-Body Balance and Endpoint Precision Control During Motor and Cognitive Dual Tasks: Effects of Cognitive Challenges in Older Adults with Cognitive Impairment of Different Severity (NSTC 2024-2027)

A. Advancing Movement Science in Orthopedics
Our research focuses on how musculoskeletal disorders and surgical interventions influence human movement and balance. Using three-dimensional motion capture and ground reaction force analysis, we investigate joint coordination, dynamic balance control, and adaptive gait control across a range of orthopedic and neuromuscular conditions.
In anterior cruciate ligament-deficient (ACLD) individuals, uphill walking was shown to reveal latent instability and compensatory neuromuscular adaptations that remain undetected during level walking, highlighting uphill walking aids clinical evaluation and informs surgical decisions in ACLD copers. Studies on developmental dysplasia of the hip (DDH) demonstrated persistent asymmetries in joint coordination and endpoint control even after early treatment, particularly in cases complicated by avascular necrosis, underscoring the need for long-term motion-based evaluation.
Research on knee osteoarthritis (OA) and total knee arthroplasty (TKA) established quantitative measures for postoperative recovery. Patients with bilateral medial knee OA exhibited impaired balance control, while those treated via the mid-vastus approach achieved faster restoration of gait stability, altered center-of-mass (COM)–center-of-pressure (COP) dynamics (Figure 3) compared with conventional lateral parapatellar techniques (Figure 4).
Extending to spinal and pediatric populations, investigations in lumbar spondylosis linked altered COM-COP dynamics to reduced gait stability, whereas studies in adolescent idiopathic scoliosis, genu valgum and cerebral palsy revealed asymmetrical balance strategies and compensatory joint stiffness regulation.
Together, these studies form a cohesive framework for understanding whole-body balance and locomotor adaptation in pathological gait. The findings advance quantitative gait analysis as a clinically applicable, evidence-based tool for improving diagnosis, surgical planning, and rehabilitation in orthopedic and neurological care.

Figure 1. Schematic diagram showing a stick figure of a typical participant during level walking showing the COM and COP, and the COM-COP vector forming the sagittal inclination angle (IA) (A) and frontal IA (B) with the vertical. The reference limb is shown in darker grey.

Figure 2. Mean curves of the COM-COP inclination angles (IA) and their rates of change (RCIA) in the sagittal and frontal planes for the knee osteoarthritis groups 3 months after TKA via LPPA (red lines) and MVA (blue lines), and the control group (black dashed lines) during level walking in the sagittal (A, B) and frontal (C, D) planes. Positive sagittal and frontal IA indicate COM positions that are anterior and contralateral to the COP, respectively. Positive sagittal and frontal RCIA indicate rates of anterior changes and contralateral changes in the corresponding IA, respectively. Heel-strike (HS), contralateral toe-off (CTO), contralateral heel-strike (CHS) and toe-off (TO) are indicated by vertical lines. IA and RCIA were temporally normalized by the stride time to be in 0%–100% of the gait cycle. Asterisks (*) indicate statistical significance (p < 0.05) between LPPA and Control, and crosses (†) indicate statistical significance (p < 0.05) between MVA and Control for the time-averaged IA or RCIA values over double-limb support (DLS) or single limb-support (SLS) phases.
B. Advancing Movement Science in Neurology
Falls are a major neurological and geriatric concern, often resulting in injury, disability, and loss of independence. Safe locomotion requires the continuous integration of sensory input, motor execution, and cognitive control. Aging and neurological disorders can disrupt this integration, leading to instability and increased fall risk. Understanding how the neuromuscular system adapts movement strategies under cognitive and sensory constraints is therefore fundamental to advancing both movement science and fall-prevention research.
Advancing movement science in neurology and fall risk focuses on identifying how motor control adapts when the central nervous system is challenged by aging, cognitive decline, or disease. Using three-dimensional motion analysis and optimal control modeling, Lu and colleagues have systematically examined how individuals modify gait kinematics and coordination when negotiating obstacles—a functional task closely related to everyday falls.
In healthy older adults, performing a cognitive-motor dual task leads to strategic kinematic adjustments, including increased toe-obstacle clearance and altered limb coordination, reflecting compensatory control to maintain safety under divided attention. Similarly, monocular viewing immediately perturbs lower-limb kinematics, emphasizing the reliance of locomotor stability on visual feedback and the heightened vulnerability of older adults to sensory degradation.
In individuals with mild cognitive impairment (MCI), attentional demands further disrupt locomotor control. Older adults with MCI exhibit altered obstacle-crossing strategies and reweight control objectives to prioritize stability and clearance over efficiency, as revealed by multi-objective optimal control modeling. These findings indicate that cognitive decline reshapes motor planning and contributes to elevated fall risk.
Studies across clinical populations reinforce this framework. Children with Duchenne muscular dystrophy employ exaggerated limb motions to compensate for muscle weakness. Patients with diabetes mellitus show trailing-limb clearance deficits linked to proprioceptive loss, and individuals with Parkinson’s disease display impaired axial coordination during turning. Even mild brain injury, such as concussion, can disrupt inter-joint coordination during divided-attention walking, demonstrating persistent cognitive–motor coupling deficits.
Together, these investigations establish a unified perspective on how the brain and body interact to preserve balance under constraint. By integrating biomechanics, neuroscience, and computational modeling, this body of work advances understanding of adaptive locomotor control across health and disease. The resulting insights support the development of objective markers and targeted interventions to reduce fall risk in aging and neurological populations.
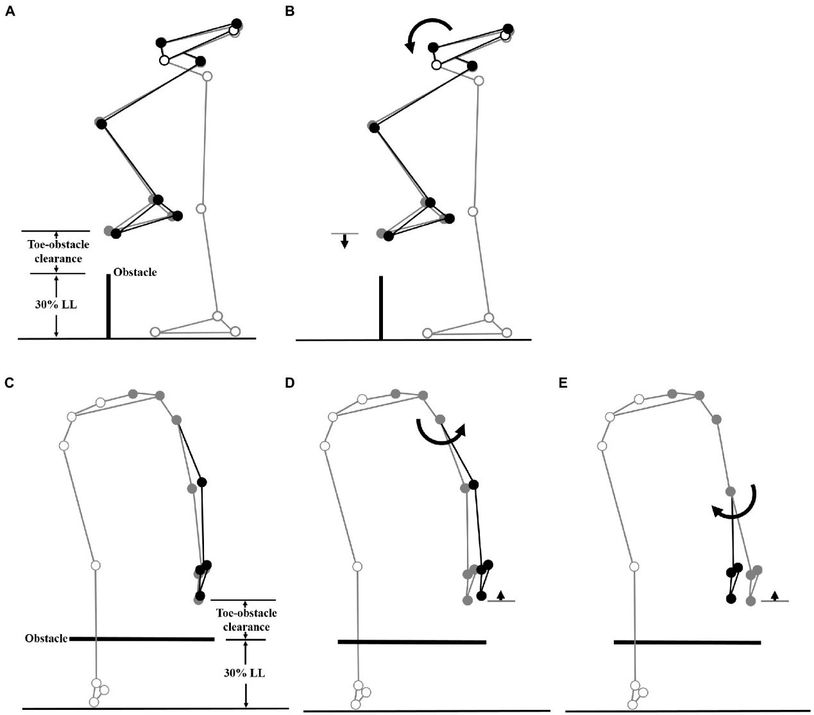
Figure 3. The planar seven-link model of the body during obstacle-crossing. Two forceplates are placed on either side of the obstacle. a Definitions of the toe-obstacle clearance and the joint angles are also indicated: hip (θ_LH), knee (θ_LK) and ankle (θ_LA) of the leading swing-limb, and foot (θ_TF), ankle (θ_TA), knee (θ_TK) and hip (θ_TH) of the trailing stance-limb. The upper body, namely the segments of the head/neck, trunk, pelvis, and upper extremities, was modeled as a single link, defined as the line connecting the hip joint center and the center of mass of all the upper body segments. The hip angles were defined as the angles between the upper body link and the thigh links. The X-axis indicates the direction of progression.
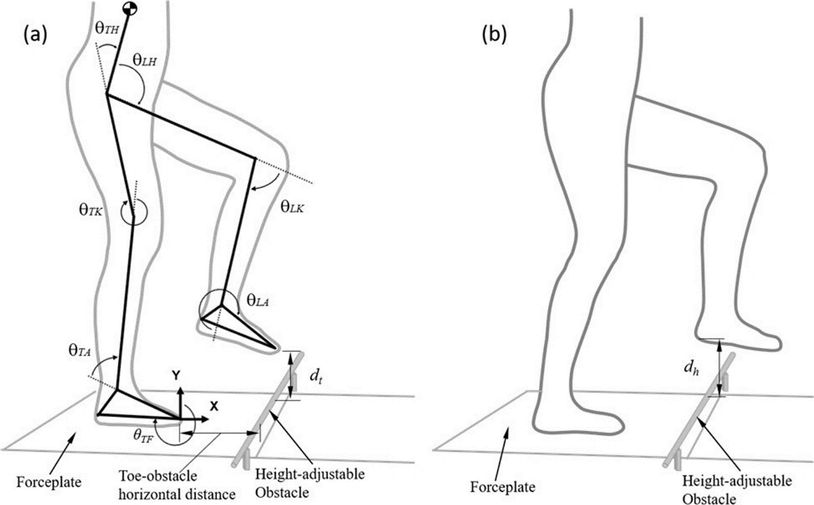
Figure 4. Effects of the observed significant angular changes at individual joints on the leading toe-obstacle clearance in the MCI group (black stick figure) compared to Control (A and C, grey stick figure) when the leading toe was above an obstacle of 30% leg length in height. The stick model was drawn using marker positions of a typical subject from each group. The segments with solid grey circles are joints of the reference limb. With the stance foot fixed to the ground, only one joint was rotated at a time, while keeping the angles of the other joints fixed, and the segments of the stance limb and the segments of the swing limb distal to the current joint stationary. The MCI group showed increased pelvic anterior tilt (B), and increased hip abduction (D) and knee adduction (E) in the swing limb. As indicated by the black stick figure, while (D, E) tended to increase the leading toe-obstacle clearance, (B) gave the opposite effect, leading to the observed normal toe-obstacle clearance.
C. Advancing Movement Science in Footwear and Environmental
Our research examines how external conditions, such as gait speed, slope, footwear design, and foot morphology, affect locomotor control, joint load distribution, and balance. Using three-dimensional motion capture and force analysis, we investigate how the body adapts dynamically to maintain stability and efficiency under changing mechanical constraints.
Studies on walking speed and environment revealed that changes in treadmill or over-ground conditions alter the coupling between the COM and COP, reflecting adaptive balance strategies that sustain dynamic stability. Research on inclined and declined walking showed that uphill gait increases hip and knee extensor loading for propulsion, whereas downhill gait shifts support toward the ankle and contralateral limb to control descent.
Investigations into footwear biomechanics demonstrated that elevated or narrow heels modify joint coordination, redistribute support moments, and alter COM-COP control. Long-term high-heel use and foot deformities such as bilateral hallux valgus were further shown to increase proximal joint stress and impair balance regulation.
Additionally, a single-image-based pin-array reconstruction method was developed to measure foot sole morphology with high reliability, enabling precise evaluation for clinical and ergonomic application.
Together, these studies establish a biomechanical framework for understanding how environmental and functional factors shape gait stability and load redistribution, informing the design of ergonomic footwear, orthotic devices, and mobility rehabilitation programs.